Thoughtful acoustic design in healthcare facilities is critical for patient healing, safety, and operational success. Yet according to “Noise and Sleep Among Adult Medical Inpatients: Far From a Quiet Night,” published in JAMA Internal Medicine, most facilities exceed the World Health Organization’s (WHO) noise recommendations by 20-plus decibel (dB), reaching sound levels on par with big-city traffic or a blender.
That noise level isn’t just a comfort issue. It’s a business risk that impacts patient recovery, staff performance and retention, and regulatory compliance.
As noise levels have increased over the past 20 years in clinical facilities, it has been shown that Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey scores for noise level were poor in many facilities, skewing overall scores downward. This alone should alert owners and designers to the importance of good acoustic design.
The solution lies in integrated acoustic design: the comprehensive consideration of sound from the project inception to optimize patient outcomes and facility performance. This proactive approach enables healthcare facility developers to deliver measurable improvements in patient satisfaction, staff performance, and operational effectiveness, while preventing costly remediation.
Integrating acoustics design across project teams
Healthcare acoustics must not be an afterthought in the design process but instead treated as core infrastructure. Optimizing acoustic design requires close collaboration between architecture, engineering, mechanical, and construction teams from day one.
Success begins with a deep understanding of how the acoustics of space can enhance or hinder the patient experience.
For example, a clinical review, “The impact of noise on patients’ sleep and the effectiveness of noise reduction strategies in intensive care units,” published in the journal Critical Care, reports that sleep deprivation during a hospital stay slows healing.
The problem is even worse for pediatric environments, with research showing that loud, unfamiliar sounds create medical anxiety that adds to the trauma and fear of the entire experience.
Early acoustics integration aims to solve issues before they develop, preventing late-stage corrections, reducing the cost and hassle of mid-construction remediation, and improving outcomes and performance of the facility.
6 design strategies to meet healthcare facility standards
In addition to the WHO guidelines, several industry organizations provide noise-related standards, including the Facility Guidelines Institute (FGI), American Society for Health Care Engineering (ASHE), American National Standards Institute/Acoustical Society of America (ANSI/ASA), U.S. Green Building Council’s LEED program, and even the Veterans Administration (VA.)
Here are six acoustic design strategies that can help achieve compliance with these industry standards and create the optimal auditory comfort patients need to maximize recovery.
- Create quiet zones. Incorporating quiet spaces in patient areas can support recovery and quality metrics by reducing medical complications. And, just like patients, providers also need breakrooms and sleeping spaces that provide respite from the cacophony of noise so that they may recharge and de-stress. Buffer spaces like storage rooms can be used to separate patient rooms and staff sleeping areas from busy or noisy spaces like nurses’ stations and public corridors. Designers can also position medication rooms, which are often bustling with activity, away from patient rooms to isolate them from the traffic noise. Also, avoid placing patient room doors directly adjacent to or across from nurses’ stations and elevators to prevent channeling these noise sources directly into patient rooms.
- Consider materials choices. The FGI’s Guidelines for Design and Construction of Health Care Facilities provides material standards for building components used in healthcare facilities that are designed to dampen sound, reduce reverberation, and provide speech privacy. Specifically, designs should specify wall materials and doors that meet these criteria with greater than 45 sound transmission class (STC) rating, ceiling tiles with noise reduction coefficient (NRC) of at least 0.85, and acoustic flooring to isolate vibration and sound transmission from levels above where appropriate. In behavioral health settings where excessive noise can trigger or exacerbate post-traumatic stress disorder, anxiety, and depression, project teams should consider tamper-resistant materials that meet these acoustic guidelines for added safety.
- Minimize alarm pollution. Incessant alarms not only disrupt patients’ rest and cause added stress, they also negatively impact staff. A study “Effect of Noise in the Emergency Department on Occupational Burnout and Resignation Intention of Medical Staff,” published in Noise & Health, found that long shifts in noisy environments can also raise staff stress, cause burnout, and reduce job satisfaction. For nurses in the intensive care units, where precision and attentiveness are vital, noisy environments are the number one performance obstacle, according to research “Performance Obstacles of Intensive Care Nurses,” published in Nursing Research. At a time when skilled professionals are in critically short supply, facilities can’t afford to lose employees over preventable acoustic issues. Technologies such as visual alarms or personal/wearable notification devices allow staff to receive targeted alarms quietly and individually rather than having them broadcast throughout the space.
- Be mindful of HVAC and mechanical noise. The FGI calls for sounds from these sources to be maintained below noise criteria (NC) 25-30 to reduce patient disturbance. The use of air silencers, duct lining and insulation, and noise-suppressing duct mounts can maintain noise levels within the recommended range. When designing duct runs, minimize bends to improve both acoustic and air flow performance. Design teams should also avoid placing mechanical equipment and vents directly above patient beds and operating and exam tables to minimize patient-adjacent noise. These strategies are especially critical in areas such as operating rooms and medication stations where excess background noise can prevent staff from accurately hearing instructions and patient details, potentially leading to medical errors or treatment delays.
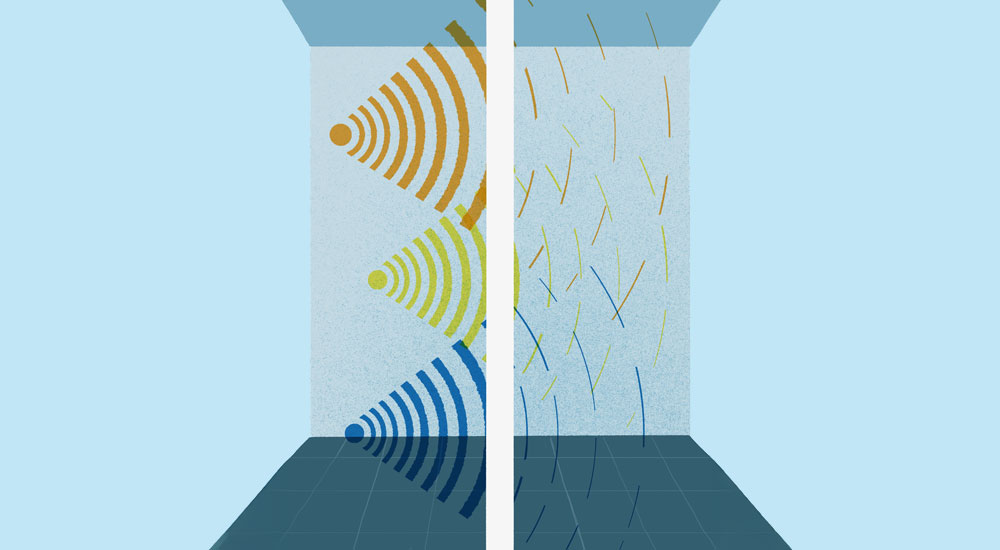
- Use strategic noise as an advantage. In areas with poor sound dampening, patients may withhold sensitive details of their situation out of fear of being overheard, which can interfere with appropriate treatment. The use of sound-masking systems that elicit low-level “white noise” can provide “cover” for voice dampening and prevent conversations from being overheard by others. It’s important to be mindful that complete silence in a medical environment can be just as unnerving as too much noise, causing patients to feel isolated and worry they’ve been forgotten.
- Give patients control. Empowering patients to control their own experience provides agency in a situation where they may otherwise feel helpless. Installing interactive room controls allows patients to create their own sound environment, such as soothing nature sounds like rainfall or ocean waves. These systems can mask unwanted noise as well as help reduce patient stress and aid in restful recovery.
Addressing acoustics through building façades, site considerations
While addressing acoustics, project teams shouldn’t overlook design considerations for building façades and facility sites. For example, in urban environments, healthcare facilities face unique challenges from traffic, construction, and emergency vehicle noise.
High-performance window systems that meet the FGI’s minimum STC 40 rating for sound proofing, strategic building orientation to minimize patient exposure to primary noise sources, and landscape design that includes natural sound barriers are viable design solutions. Prefabricated façade design should factor in noise and vibration isolation during the design and specification phase.
Integrating biophilic design throughout the facility can also offer dual benefits. Natural elements like living walls, water features, and organic wallcovering materials such as natural wood slats with acoustic backing, cork panels, or bamboo can have synergistic benefits: Natural materials offer superior sound absorption compared to synthetic alternatives, while the soothing aesthetics reduce stress and promote healing.
While integrating acoustic design into a new build is simpler than retrofitting, existing facilities can still take steps to improve their sound environments. Healthcare facilities frequently undergo renovation, which provides an opportunity to address acoustics.
During this process, project teams should perform an analysis of acoustic conditions prior to any changes to find areas for improvement and establish an empirical baseline.
Impact of robotics, materials selection on sound in healthcare facilities
As in every design process, it’s essential to think about future needs and opportunities. In healthcare, project teams should consider the rise of robotics and automation in the healthcare space and its impact on the care environment. Planning acoustic design now for these advances can help maintain a comfortable environment even as autonomous technology becomes more commonplace.
For example, when selecting autonomous mobile robots, project teams should pay attention to the sounds the equipment makes when performing various functions and choose models with adjustable volume and mute options. Robotic delivery to patient bedside will require consideration for powered door operators and related annunciators to create a pleasant patient experience.
Similarly, balancing cost and efficacy must remain a priority in future-ready design.
While the use of modern, prefabricated components can speed construction for both new builds and renovations, these elements must be compatible with acoustic standards. Design teams should factor in sound leakage and dampening for prefabricated component installation such as caulking, isolation pads, fastening and mounting methods.
Fortunately, advances in material science such as composite panels that incorporate foam, mineral wool or polymers, and microperforated surfaces to dissipate sound are making this approach both effective and affordable.
Prioritizing acoustics in healthcare design
Sound has a tangible impact on facility performance and profound effects on patient outcomes.
Developers and design teams that prioritize acoustics in the earliest design phases will deliver facilities that leverage sound as a strategic advantage to support healing rather than hinder it.
Steven Goldfarb is an information and communications technology discipline leader at HED ( Los Angeles) and can be reached at [email protected]. Bruce Macpherson is a healthcare sector leader at HED (Los Angeles) and can be reached at [email protected].